Image Courtesy of CADRE
Clinic 20XX: Designing for an Ever-Changing Present (A COVID Era Study)
RESEARCH TEAM
Upali Nanda, Deborah Wingler, Rutali Joshi, Daniela Aguirre Alfaro, Melissa Hoelting
FUNDS
CADRE and HKS Inc.
Scroll to the bottom of page to download full report.
primary care in the pandemic era
The rising cost of healthcare has been an ongoing concern for policy makers, healthcare providers, and patients. In a 2014 Commonwealth report, the U.S. spent the most on healthcare, compared to 10 other developed countries, while the quality of care was rated among the lowest. When this study was repeated in 2021, our ranking as a country had not changed. Meanwhile, countries like Norway and Netherlands had moved significantly higher in raking on the key indicators: quality of care, equity, efficiency, healthy lives, and access.
What are we missing in the way we are doing things? There is an urgency for healthcare organizations, patient advocates, and policy makers to change healthcare and bring about systemic and system-wide reform. The challenges with COVID-19, the rise in our health worker burnout, and the fundamental issues with public health bring onto sharp relief the future (and present) of outpatient care today.
The CADRE and HKS team studied how the world of primary care had changed from the Clinic 20XX research from 2015, in large part due to the pandemic. The purpose for this Clinic 20XX refresh was to:
Revisit key drivers and trends
Observe changes in primary care expectations from the patient’s perspective by generation (Millennial, Gen X, Baby Boomer)
Observe changes in primary care from the physician’s perspective
emerging drivers and trends
We identified new key drivers and trends, in addition to the ones from 2015 that continue to be relevant. Read more about them on pages 3-6. Emerging drivers of change included:
Climate Change (Respiratory Diseases, Catastrophic Events): The health effects of the long-term climate shift’s we are seeing include respiratory and cardiovascular disease, injuries and premature deaths related to extreme weather events, water-borne illness, other infectious diseases, and threats to mental health.
Burnout (Staff Burnout and Retention, Mental Health): Healthcare worker burnout is at an all-time high, especially in primary care physicians, nurses, and care team attributed in large part to the unique stresses of the last two years including unprecedented financial strain.
Infectious Diseases (Global Outbreaks): The growth in global connectivity (coupled with the rapid changes in demographics), climate, and technology have ushered an era of infectious disease outbreaks at unprecedented scales, despite significant improvements in sanitation and health.
Health Equity (Access to Care, Treatment Availability, Outcome): The disproportionate impact of COVID-19 on various socio-economic groups, coupled with an increased sensitivity to equity with the political events of the last two years, make health equity (in terms of access to quality care) a fundamental driver of primary care today.
In response to the existing and emerging drivers we identified some key emerging trends which included:
New Players in Market (Empowering Customers, Removing Traditional Barriers): New entrants from outside the traditional healthcare industry, like Apple, Google, and Amazon, are redefining primary care and bringing customer-centric, innovative business and care models to provide more affordable, convenient care options focused on health and wellness.
Wellness (Focus on Exercise, Nutrition, Sleep and Mental Health): In a growingly health-conscious society, consumers spend significantly to take care of their body and mind. Wellness amenities are seen as the differentiating value proposition for many primary care clinics, with a potential shift in the role of the primary care team from a provider to a life-partner around health and wellness.
Home Health (Convenient Health Services at Home): With the rapid acceleration of telehealth, an increasing aging population, and extreme advancements in medical technology, the need and the range of services that can be provided directly at home have only increased and will only increase due to the long-ranging effects from COVID-19.
Survey: patients and physicians
WHAT DID WE DO | HOW DID WE DO IT
We commissioned an unbiased, third-party independent vendor to survey U.S. patients and physicians on their primary care experiences and preferences, including both telehealth and in-person clinic visits. Survey respondents include:
330 patients (110 Millennials, 110 Gen X, and 110 Baby Boomers) who had a telehealth visit in the last nine months for primary care needs (January 2021)
103 physicians (60 Family Practice and 43 Internal Medicine) who transitioned to or expanded telehealth services during the COVID-19 crisis (May 2020)
Changing patient expectations from primary care: a generational perspective
WHAT DID WE FIND
As COVID-19 eased, patients began to return to the clinic for in-person visits at the end of 2020 through the beginning of 2021 at increased volumes: 51% had an in-person clinic visit in the past six months (surveyed between January and March 2021). Overall, the top three components of an ideal clinic experience for primary care in-person were identified as:
1. Streamlined process (44%)
2. Empathetic & Knowledgeable providers (27%)
3. Amenity-rich, safe, and clean environment (21%)
Overall, Patients saw themselves as patients needing health services (78%) more than as consumers buying health services (22%).
Respondents were generally open to sharing data for care continuity (58%). In fact, more trust was placed in information (57%) than in people (43%) [This is a shift from 2015 when trust in people trumped trust in information, and was especially true for Gen Xers].
While some trends transcend generations, there are some generational preferences that are good to be aware of.
For example, Boomers consider their phones only as a means of communication (60%) rather than as a lifeline (40%) - in sharp contrast to Millennials and Gen Xers.
Boomers also preferred in-person visit (70%) over virtual visit (30%), whereas Millennials preferred virtual visits (58%) compared to in-person, and Gen Xers were on the fence but leaning towards in-person (55%). This finding will be interesting to check a few years post-COVID to understand the “COVID-effect”.
Top two factors across all generations were Health Plan Coverage and Cleanliness. However on-site diagnostics were much more important to Baby Boomers and Gen-Xers. Digital convenience was more important for Millennials. Read page 15-20 to see the top factors for selection and appeal across generations.
Changing physician expectations from primary care
WHAT DID WE FIND
Physicians reported being satisfied with their practice today (avg. 4.0 out of 5 stars) and highlighted patient relationships (4.57 rating out of 5 and mentioned most frequently in free text response) to be key for success. Top facility features that help physicians run a successful practice were identified as:
streamlined patient check-in and registration process (4.58 out of 5) and
availability of exam room when needed (4.56 out of 5)
Overall, physicians want less regulation, more time with patients, and more integrated information systems. COVID-19 has pushed even more time away from the patients on administrative tasks and primary care physicians value the patient relationship which is at risk. While excited about telehealth, physicians are still skeptical about the regulatory reform needed to make it successful.
MOVING FORWARD
WHAT IS NEXT | WHAT DOES THIS ALL MEAN TO US AS A DESIGN THINKING COMMUNITY?
Patients first. Consumers second. A choice-based, consumer-centered focus is relevant, but only when focused on the foundational needs of patients. This means less attention to bells and whistles, and more attention to health, wellbeing, clinical effectiveness and overall experience.
Coverage, cleanliness, and convenience set the foundation of a successful primary care experience. Convenience means different things to different generations. For Boomers it is about on-site diagnostics, while for Gen Xers and Millennials it is also about on-site medications, less than 30-min wait, and distance from home.
Digital experience defines satisfaction with in-person visit. While rating in-person experiences, patients still mention digital convenience like online registration and mobile apps.
The ideal clinic experience is defined by a seamless process that spans digital and physical entry points, empathetic and knowledgeable-providers, and amenity-rich and clean environments. In the last six years there has been a shift from on-site amenities (like a spa-like atmosphere and on-site retail) to digital amenities like health-tracking mobile apps.
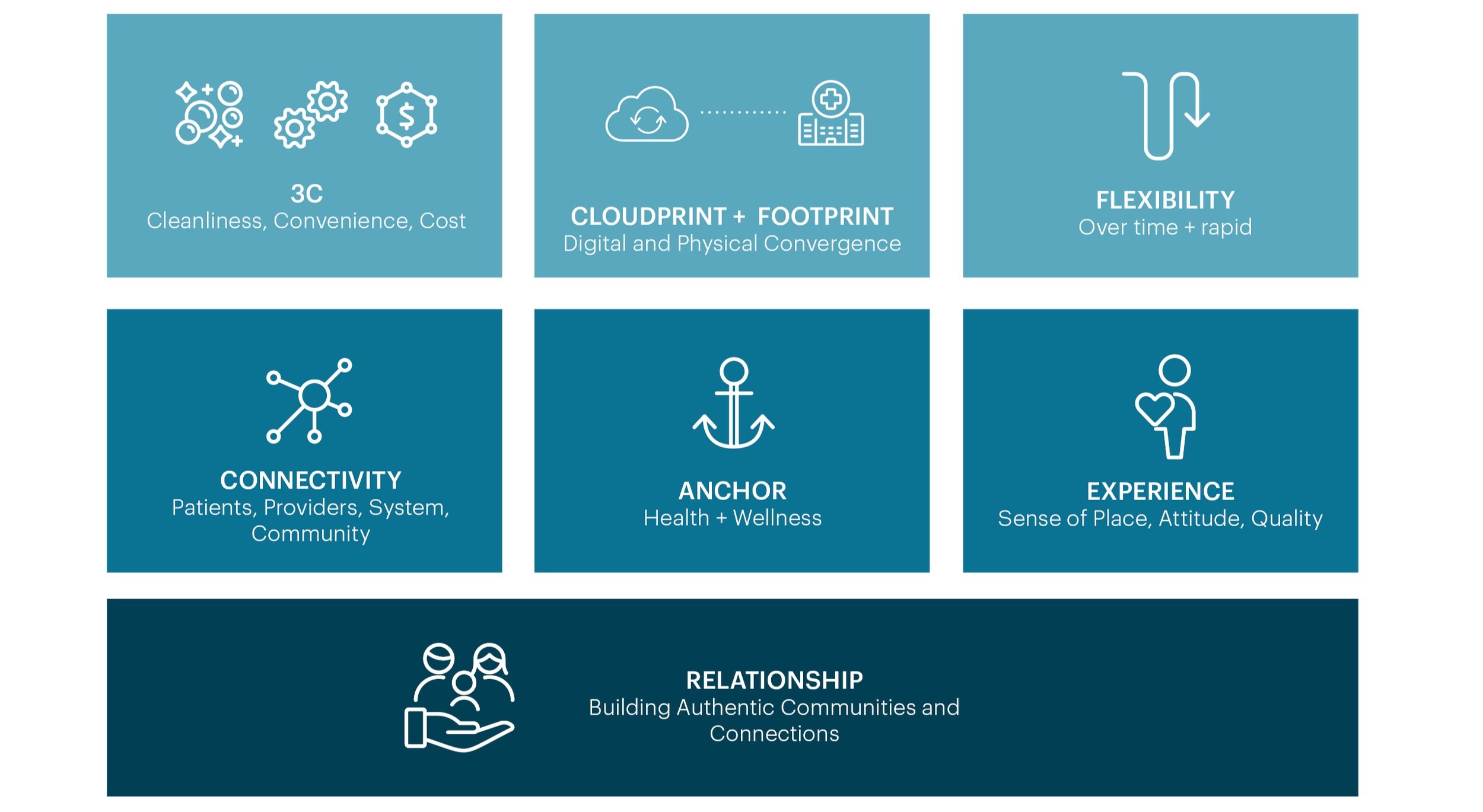
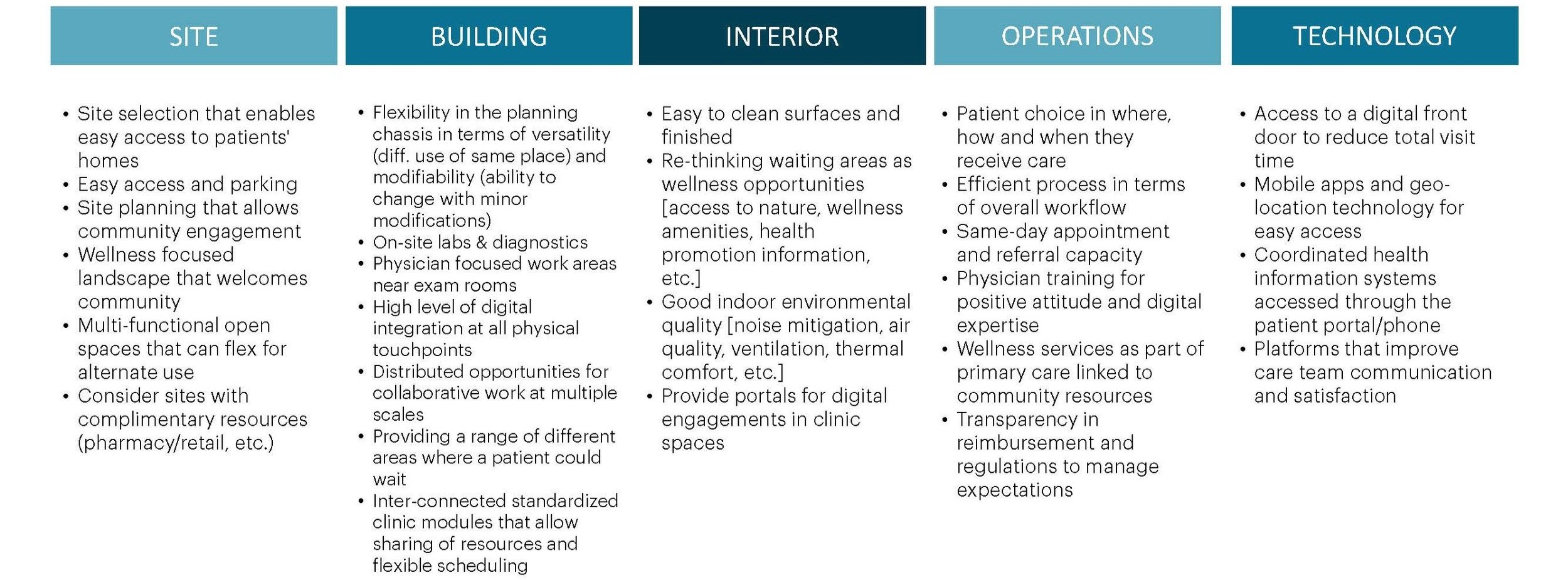
We developed seven key principles to design primary care clinics that are change-ready from layering patient and provider perspectives on the key drivers and emerging trends. These principles can then be translated to implications for site, building, interior, operations, and technology design. (Access the full implications on page 39-40.)
Seven Key Principles:
Design Implications
The pandemic brought into sharp relief some of the systemic issues that were underpinning our challenges in healthcare. The lived experiment of the pandemic has once again reinforced the need for change-ready facilities.
This study concluded what has been six-year exploration of how to design for change in the face of an ever-changing present. It is our hope that others will take the insights from this report, continue to ask questions, and use it as a starting point for meaningful innovation.